Lifestyle and Healthy behaviours
24 Hour Physical Behaviours
The importance of physical activity for people living with type 2 diabetes is well known.
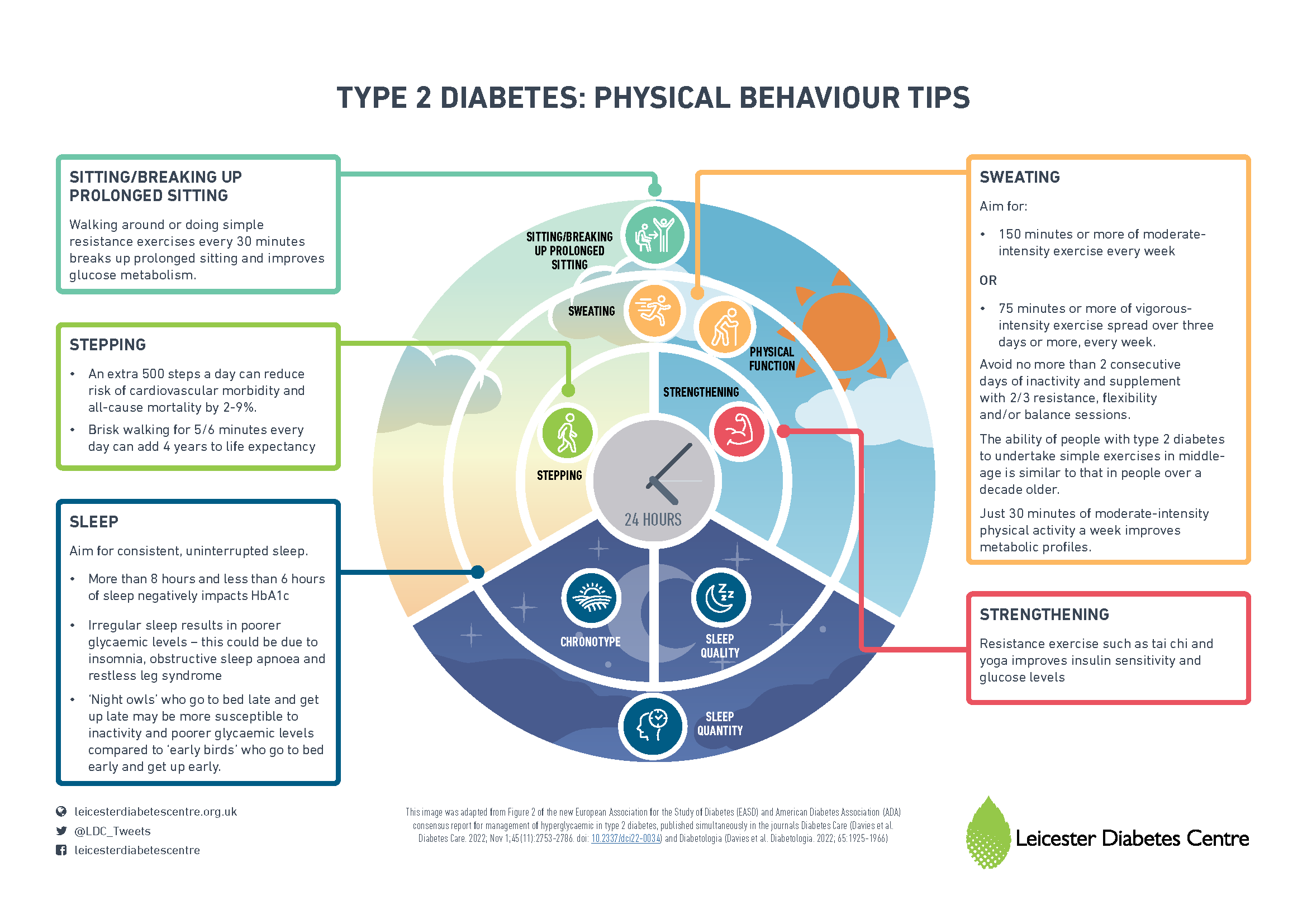
For the first time, the importance of physical activity and sleep across the whole, 24 hour day has been recognised within the recent European Association for the Study of Diabetes (EASD) and the American Diabetes Association (ADA) consensus report.
The Leicester Diabetes Centre identified five important physical behaviours included in the guidelines, which people with diabetes should be aware of to help them better manage their condition. The five important physical behaviours published in the guidance include the five S’s: Sitting, Stepping, Sweating, Strengthening and Sleep. You can see this outlined in more detail in the figure across.
It is essential to be aware of how important the whole day is when talking about activity levels and health. The animation across explains this in more detail.
Watch the video from Professor Davies and members of the Leicester Lifestyle and Health Research Group based at the Leicester Diabetes Centre, who undertake work to change and improve international guidance on physical activity and for people living with long-term conditions. The video has more of an in-depth look at the five S’s and how these affect our day to day lives.
The research from the Leicester Diabetes Centre which informed the 5S’s below can be found below
Dempsey PC, Larsen RN, Sethi P, Sacre JW, Straznicky NE, Cohen ND, et al. Benefits for Type 2 Diabetes of Interrupting Prolonged Sitting With Brief Bouts of Light Walking or Simple Resistance Activities. Diabetes Care 2016 Jun;39(6):964-972.
Henson J, Rowlands AV, Baldry E, Brady EM, Davies MJ, Edwardson CL, et al. Physical behaviors and chronotype in people with type 2 diabetes. BMJ Open Diabetes Res Care 2020 Jul;8(1):10.1136/bmjdrc-2020-001375.
Yates T, Haffner SM, Schulte PJ, Thomas L, Huffman KM, Bales CW, et al. Association between change in daily ambulatory activity and cardiovascular events in people with impaired glucose tolerance (NAVIGATOR trial): a cohort analysis. Lancet 2014 Mar 22;383(9922):1059-1066.
Rowlands A, Davies M, Dempsey P, Edwardson C, Razieh C, Yates T. Wrist-worn accelerometers: recommending ~1.0 mg as the minimum clinically important difference (MCID) in daily average acceleration for inactive adults. Br J Sports Med 2021 Jul;55(14):814-815.
Kraus WE, Yates T, Tuomilehto J, Sun JL, Thomas L, McMurray JJV, et al. Relationship between baseline physical activity assessed by pedometer count and new-onset diabetes in the NAVIGATOR trial. BMJ open diabetes research & care 2018 Jul 19;6(1):e000523.
Jelleyman C, Yates T, O'Donovan G, Gray LJ, King JA, Khunti K, et al. The effects of high-intensity interval training on glucose regulation and insulin resistance: a meta-analysis. Obes Rev 2015 Nov;16(11):942-961.
Mickute M, Henson J, Rowlands AV, et al. Device-measured physical activity and its association with physical function in adults with type 2 diabetes mellitus. Diabet Med. 2020:e14393
Nutrition Therapy
Medical nutrition therapy
Recommendations promote and support heathy eating patterns. There are two core approaches which positively impact management of diabetes and glycaemic control:
Weight management including weight loss and maintenance
Diet quality including management of carbohydrates
1. People living with overweight or obesity should be encouraged to consider weight loss approaches
If weight loss is a goal, then dietary restriction, lifestyle and/or other treatments should be agreed as part of shared decision making.
Figure 1. Benefits of weight loss depend on starting weight and level of weight loss achieved.
Figure 1. illustrates the continuum of weight loss with potential benefits. 5-10% weight loss can confer cardiometabolic improvements including reducing blood pressure and risk of heart disease. Greater weight loss can lead to improvements in disease symptoms, progression and even lead to remission of type 2 diabetes. The method of weight loss will impact the level of weight loss than can be achieved. Behavioural diet and lifestyle approaches can achieve 0-10%, pharmacotherapy plus lifestyle or surgery 15% and more. Choice of glucose lowering therapies is important for weight loss and maintenance.
Figure 2. Achievement and Maintenance of Weight Management Goals:
Figure 2. No single weight loss approach will suit everyone and individualised person-centred targets should be set.
Lifestyle and behavioural programmes including 24-hour physical behaviour change can support people to achieve weight loss goals e.g. structured weight management programmes. These complement other treatments and can provide additive weight loss e.g. lifestyle plus glucose therapy. People should be offered options for online, virtual, 1-2-1, in person and group programmes to suit their needs and preferences. Cultural adaptation of programmes, peer and/or social support are important for weight loss and long-term maintenance of weight loss. Individual goal setting and monitoring will support motivation.
2. Diet quality can impact glycaemic control and health risks
There is no single ratio of carbohydrate, fat and protein which works best for everyone with type 2 diabetes. Recommendations include optimising foods that impact health for the individual e.g. improve glucose control. Changes should be led by the individual and accommodate preferences and individual goals to help make them sustainable, while aiming to maintain a variety of food and drink.
Day to day glycaemic control can be improved through modification of carbohydrate intake. Reducing carbohydrate foods or sugary drinks can be a straightforward option as they can be easily identified by most people. Also, changing easily digestible carbohydrates e.g. white bread, pasta and rice, to higher fibre options e.g. wholegrain. Carbohydrate reduction should be managed in line with an individual’s therapies.
Other dietary aims are to reduce increased risks for heart disease, including high blood pressure. These should be prioritised on an individual basis and follow national guidance, e.g. American Heart Association 2021 Dietary Guidance to Improve Cardiovascular Health.
Person-centred care should facilitate healthy behaviours and weight management
Figure 3. has four points for integrating medical nutrition therapy (MNT) and diabetes self-management education and support (DSMES), into clinical management of people with type 2 diabetes. Shared decision making, self-monitoring and complementary glucose therapies all support individualised approaches to nutrition therapy and weight management that can lead to sustainable behavioural change.
Figure 3. Facilitating Healthy Behaviours and Weight Management
The full ADA/EASD Consensus Report 2022 can be accessed here: https://diabetesjournals.org/care/article/45/11/2753/147671/Management-of-Hyperglycemia-in-Type-2-Diabetes